Disclaimer: This web page was produced as an assignment for an undergraduate course at Davidson College.
Nanopore sequencing of clinical blood samples in Ghana revealed gene variants linked to anti-malarial drug resistance and identified variations in vaccine targets.
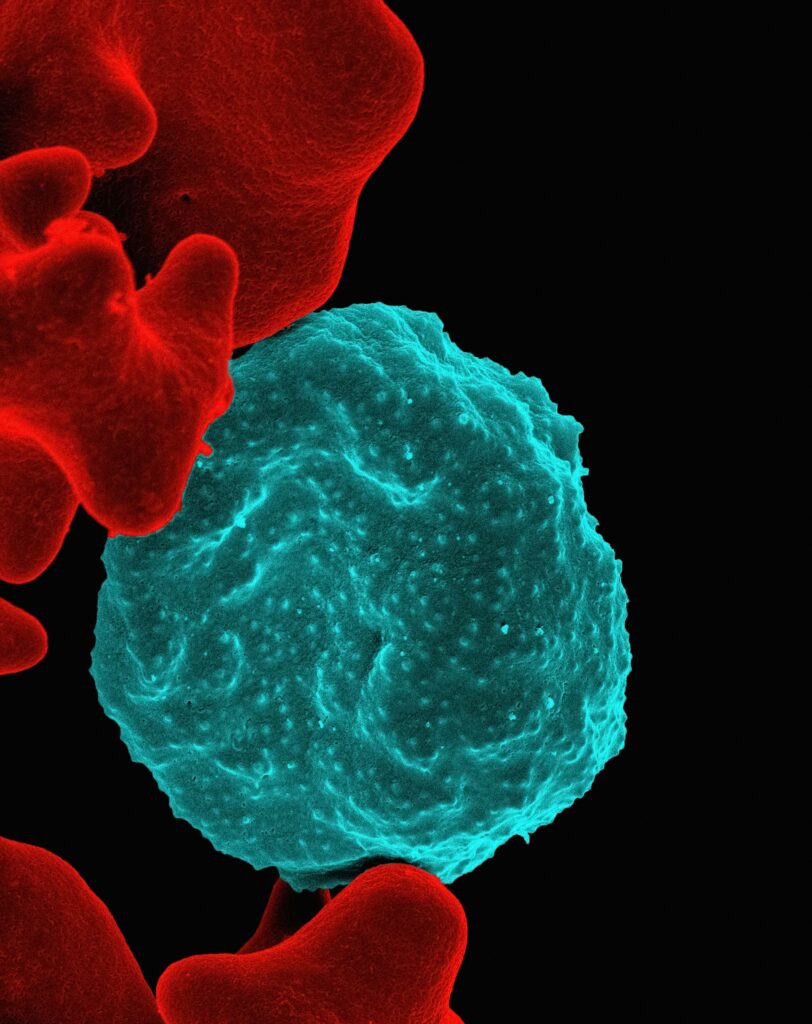
Malaria is a life-threatening disease transmitted through mosquitos, primarily prevalent in tropical countries. According to WHO, malaria caused more than 1 million global deaths in 2021 and 2022.1 Sub-Saharan Africa is largely susceptible to malaria accounting for more than 90% of the global cases and deaths in 2022. Plasmodium falciparum is a unicellular protozoan transmitted by the female Anopheles mosquito and is the leading cause of mortality.2 Upon mosquito bites, sporozoites, forms of the malaria parasites, enter the bloodstream of human beings and invade red blood cells (RBC) increasing parasite numbers. Some of the clinical symptoms of this phenomenon are fever, chills, seizures, and difficulty breathing.
Image courtesy for National Institute of Allergy and Infectious Diseases
Artemisinin is an anti-malarial drug that kills parasites by degrading one or more essential proteins. 3 Artemisinin-based combination therapy (ACT) is the most common treatment for Plasmodium falciparum. Combination therapy is the practice of combining a drug with other similar drugs to reduce the risk of developing resistance. However, mutations in people’s genomes result in drug resistance, characterized by delayed clearance of the parasites. This severely affects the effectiveness of the treatment and is especially detrimental in sub-Saharan Africa.
Comprehensive and ongoing surveillance is essential to study the genes and regions responsible for anti-malarial drug resistance. This is important to make effective alterations to malaria treatments and control policies. Previous studies proved the presence of mutations in target genes such as kelch13 and dhfr that resulted in artemisinin partial resistance.4 Here, scientists utilized nanopore sequencing to carry out genomic surveillance of antimalarial resistance in clinical malaria samples in Ghana. This sequencing technique provides long reads of DNA sequences using advanced Oxford Nanopore Technology (ONT) chemistry, achieving over 99% accuracy.
Blood samples for this study were collected in LEKMA Hospital, Accra, and three rural sites in and around Navrongo, Ghana. All 142 (100 from Navrongo and 42 from LEKMA) samples collected were positive for P. falciparum rapid diagnostic test (RDT), which validates the presence of the parasites. However, only 109 of the samples had a sufficient amount of parasites needed for the nanopore sequencing and continued to be used in the study. This study also analyzed 87 additional dried blood spot samples (DBS) collected from patients in 2018 with positive RDT in Navrongo. The median number of parasites for the DBS samples was 713 per 200 white blood cells, which is substantially lower than the venous blood samples. After obtaining a sufficient amount of data on DBS nanopore sequencing, the researchers proved that ONT is a viable method for sequencing P. falciparum directly from DBS samples.
A single nucleotide polymorphism (SNP) is a common genetic variation that results when one nucleotide in a DNA sequence changes. SNP analysis is used to study differences in the genome at an individual and societal level. This study used SNP analysis to determine anti-malarial drug susceptibility and resistance in clinical blood samples. More than 99% of the VB and DBS samples were susceptible to chloroquine, an antimalarial drug. The alleles dhfr-108N and dhps-437G exhibited 93.4% and 90.3% resistances for the drugs pyrimethamine and sulfadoxine respectively.
Common haplotypes (set of genomic variations inherited together) in target genes dhfr and dhps, are responsible for the resistance against pyrimethamine and sulfadoxine. 83.2% and 8.6% of the samples possessed triple and double mutants in dhfr respectively. Two major haplotypes were identified in dhps with 40.8% and 37.2% abundance. The mutations in the kelch13 gene, previously associated with drug resistance, were not identified in the clinical samples. This study also revealed several other concerning mutations such as dhps-581G and dhps-613S that lead to anti-malarial drug resistance.
The circumsporozoite (csp) protein is an attractive candidate for vaccination against malaria. This study investigated SNP diversity in the C-terminus of csp, the region of the vaccines RTS, S/AS01, and R21-MM target. High-frequency SNP differences from the vaccine reference sequence were identified in the analysis. For example, the 301N mutation appeared in more than 50% of the samples. Only 9% of the samples were fully similar to the vaccine sequence, which indicates the vaccine effectively targets only a minority of the overall population. The comprehensive analysis shows the feasibility of employing nanopore sequencing for targeted malaria molecular surveillance.
Ongoing surveillance to identify variants leading to antimalarial drug resistance is important to enhance clinical treatment and prevention of malaria. The above study conducted only in a small set of clinical samples in parts of Ghana, revealed variants associated with anti-malarial drug resistance. Future studies might focus on elucidating the role of these and numerous unstudied variants in anti-malarial resistance and finding potential ways to tackle them. These studies can also broaden their range of clinical samples from asymptomatic to highly severe malaria cases, which was a limitation in this study.
Implementation of such a genomic study in underrepresented regions is fundamental to making the field more inclusive and accurate. It will also enhance clinical and research practices by increasing representative clinical data. This is valuable in narrowing the health disparities persisting in the current medical field. It is also essential to ensure that the benefits of medical advancements and research are being shared equitably. Finally, such studies can also boost the trust of underrepresented communities in the medical field.
References
1. Fact sheet about malaria. https://www.who.int/news-room/fact-sheets/detail/malaria.
© Copyright 2022 Department of Biology, Davidson College, Davidson, NC 28036.
Author: Dagi Lulseged
Email: dalulseged@davidson.edu
I am very shocked at the findings of the study and the extremely high level of resistance that these drugs have. I am wondering how to make a feasible treatment for malaria, and I am wondering if we can do something similar as to what we are reading in the COVID-19 Boston paper, where they basically trace back the ancestries to understand the spread of the disease, but also how fatal it will be. While this study focuses on the drug resistance, it would be important to make a study where both the genome of malaria and the genome of the drugs are compared so an effective antagonist can be created. Thank you for your insights, Dagi!
Sickle-cell anemia is a common case study that comes up when discussing malaria and areas where it is common. I am interested to know how being heterozygous or homozygous for the sickle-cell trait may interact with the Artemisinin treatment when an individual contracts malaria. Since heterozygosity of the sickle-cell trait can provide some resistance to malaria, it may be valuable to investigate the function of Artemisinin in individuals who have this trait and how it interacts with some of the genes of interest identified in this study which cause resistance to the drug. Awesome break-down of an interesting article, Dagi!
Sickle-cell anemia is a common case study that comes up when discussing malaria and areas where it is common. I am interested to know how being heterozygous or homozygous for the sickle-cell trait may interact with the Artemisinin treatment when an individual contracts malaria. Since heterozygosity of the sickle-cell trait can provide some resistance to malaria, it may be valuable to investigate the function of Artemisinin in individuals who have this trait and how it interacts with some of the genes of interest identified in this study which cause resistance to the drug. Awesome break-down of an interesting article, Dagi!
Sickle-cell anemia is a common case study that comes up when discussing malaria and areas where it is common. I am interested to know how being heterozygous or homozygous for the sickle-cell trait may interact with the Artemisinin treatment when an individual contracts malaria. Since heterozygosity of the sickle-cell trait can provide some resistance to malaria, it may be valuable to investigate the function of Artemisinin in individuals who have this trait and how it interacts with some of the genes of interest identified in this study which cause resistance to the drug. Awesome break-down of an interesting article, Dagi!
For anyone who hopes to find valuable information on that topic, right here is the perfect blog I would highly recommend. Feel free to visit my site Article Star for additional resources about File Converters.
Awesome page with genuinely good material for readers wanting to gain some useful insights on that topic! But if you want to learn more, check out YV6 about Thai-Massage. Keep up the great work!