This web page was produced as an assignment for an undergraduate course at Davidson College. Learn more about the author
Non-malarial febrile illness (NMFI), characterized by fever, is frequently attributed to bacteria like Borrelia. Failure to diagnose NMFI in low- and middle-income countries fosters bacterial and pathogenic resistance to medications, exacerbating disease transmission.
Non-malarial febrile illness (NMFI) refers to a fever (elevated body temperature) that is not caused by malaria. This condition can stem from various sources, including viral infections (such as Zika and influenza) and bacterial infections (such as bacterial pneumonia and typhoid fever). In regions where malaria is prevalent, distinguishing between malarial and non-malarial febrile illnesses is essential for effective management and preventing complications.
To better understand the causes and treatment of NFMI in Senegal, Levine and colleagues (primary authors) collected data from febrile individuals (those who had fever at the time of study) and healthy controls (those without any signs of illness)1. Blood samples were taken from the 163 participants to identify infectious agents (e.g., viruses, bacteria), and additional data like the participants’ medical history and demographics were recorded. The study was conducted in a region of Senegal where malaria is not as prevalent as in other areas. The authors used 16S sequencing (a technique used to identify bacterial species present in a sample by targeting the 16S ribosomal ribonucleic acid (rRNA) gene) and untargeted sequencing (a method where the entire genetic material present in an individual is sequenced without selection of specific genomic regions) to test the presence of pathogens (any organism that causes disease) linked to febrile illness.
Rapid Diagnostic Tests (RDTs) for malaria were administered to each febrile patient to identify the presence of malaria parasites in their blood. Febrile cases were evenly distributed between children and adults, although there was a higher proportion of male febrile cases. Following sequencing, researchers identified viral, bacterial, and eukaryotic pathogens. The prevalence of malaria among febrile patients was notably higher during the wet season compared to the dry season in the studied population. This disparity could be attributed to several factors, including the heightened abundance of mosquitoes during the wet season, facilitated by breeding sites like stagnant water. Borrelia, a type of bacteria associated with various human diseases, emerged as the most frequently detected pathogen among febrile patients, irrespective of the season (dry or rainy) or the outcome of the malaria rapid diagnostic test (positive or negative).
Why should I care about this research?” is a relevant question. The researchers uncovered crucial insights into diagnosing and treating febrile illnesses, particularly in low- and middle-income countries (LMICs) where healthcare resources are often limited. Borrelia infections, such as Lyme disease, manifest with diverse symptoms like fever, joint pain, and neurological issues.
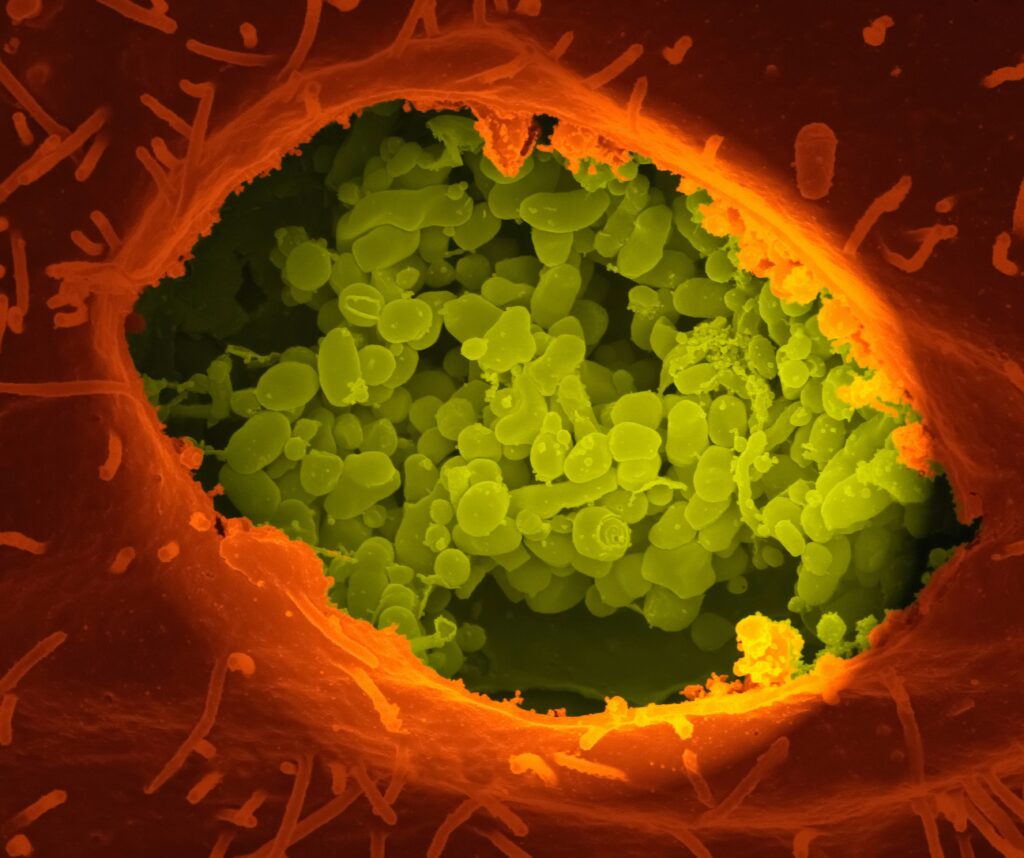
Image credit: National Institute of Allergy and Infectious Diseases
Recognizing these symptom patterns can aid healthcare providers in identifying individuals at risk of Borrelia infection. In many LMICs, healthcare facilities face constraints in accessing specialized diagnostic tests for infectious diseases like Borrelia infections. Consequently, healthcare providers often resort to Rapid Diagnostic Tests (RDTs) as the primary diagnostic tool for febrile illnesses. While these tests offer quick results and are cost-effective, they occasionally yield false negatives—mistakenly indicating the absence of a condition—impacting disease transmission.
Patients testing negative for malaria via RDTs may receive broad-spectrum antibiotic treatment, mainly when the cause of fever is uncertain. While this approach may seem economical, it can foster antibiotic overuse, exacerbating antimicrobial resistance (AMR). Antimicrobial resistance occurs when bacteria develop heightened resistance to antibiotics due to their overuse. So, what drives antimicrobial resistance? Poor hygiene, lack of education in the general population, especially in low- and middle-income countries, and rampant use of antibiotics in animal husbandry and agriculture are all major contributors to the emergence of antimicrobial resistance as a global health concern2. When a patient infected by a drug-resistant strain gets admitted to the hospital, it is primarily a cause for introducing drug-resistant organisms into a healthcare setting; these resistant organisms can transmit from one individual to the other3.
Furthermore, the findings of this study underscore the significant role of arthropod-borne bacterial pathogens, particularly Borrelia species linked with fever, as notable causes of NMFI. Despite their significance, such pathogens are hardly identified and treated as frequently as their occurrence warrants. The prevalence of bacterial pathogens uncovered in the study aligns with prior findings from targeted studies in other regions of Senegal, suggesting their potential widespread presence in Senegal and West African countries.
Underdiagnosis of these pathogens may stem from various factors, including limited awareness among healthcare providers and the absence of practical diagnostic tools. This study highlights the pressing need for heightened healthcare attention in developing countries. Due to deficiencies in medical equipment, income disparities, and educational limitations in such settings, individuals with non-malarial febrile illness may go undiagnosed, significantly affecting disease management. Moreover, the indiscriminate use of inexpensive antibiotics exacerbates antimicrobial resistance, rendering disease treatment challenging as these drugs become less effective over time.
One might inquire, “How can non-malarial febrile illness be controlled?” One approach involves bolstering access to healthcare services, especially in rural and underserved regions, to facilitate early detection, diagnosis, and treatment of NMFI. This encompasses establishing healthcare facilities, training providers, and enhancing transportation infrastructure to make healthcare more accessible. Establishing robust surveillance and reporting systems is another crucial strategy—such systems aid in monitoring the prevalence, trends, and distribution of NMFI. Timely data collection empowers public health authorities to identify outbreaks and track emerging pathogens linked to non-malarial febrile illness. Improving access to clean water, sanitation facilities, and hygiene education is pivotal in preventing waterborne and foodborne infections, thereby reducing the incidence of NMFI caused by bacterial and parasitic pathogens.
References
- Levine Z. C., A. Sene, W. Mkandawire, A. B. Déme, T. Ndiaye, et al., 2024 Investigating the etiologies of non-malarial febrile illness in Senegal using metagenomic sequencing. Nature Communications 15. https://doi.org/10.1038/s41467-024-44800-7
- O’Neill J., 2016 Tackling drug-resistant infections globally: final report and recommendations. https://apo.org.au/node/63983
- Sharma A., A. Singh, M. A. Dar, R. J. Kaur, J. Charan, et al., 2022 Menace of antimicrobial resistance in LMICs: Current surveillance practices and control measures to tackle hostility. Journal of Infection and Public Health 15: 172–181. https://doi.org/10.1016/j.jiph.2021.12.008
© Copyright 2022 Department of Biology, Davidson College, Davidson, NC 28036.
The topic of viral diseases affecting underserved populations has always been interesting to me. Growing up, I remember the spread of the Zika virus throughout Colombia. It happened extremely fast in low-income areas, where poor infrastructure, like stagnant water and a lack of access to disinfection methods, were the norm. I imagine several African countries often go through similar situations, as every new virus comes along. It was interesting to learn about how that same lack of infrastructure, in underdiagnosis and prescription of common drugs, leads to higher antibiotic resistance in these viruses. It seemed counterintuitive at first. This article does a great job of highlighting how the first step to treating viral infections in low-income populations is simply access to better care and living conditions. Not doing so, is counterproductive.